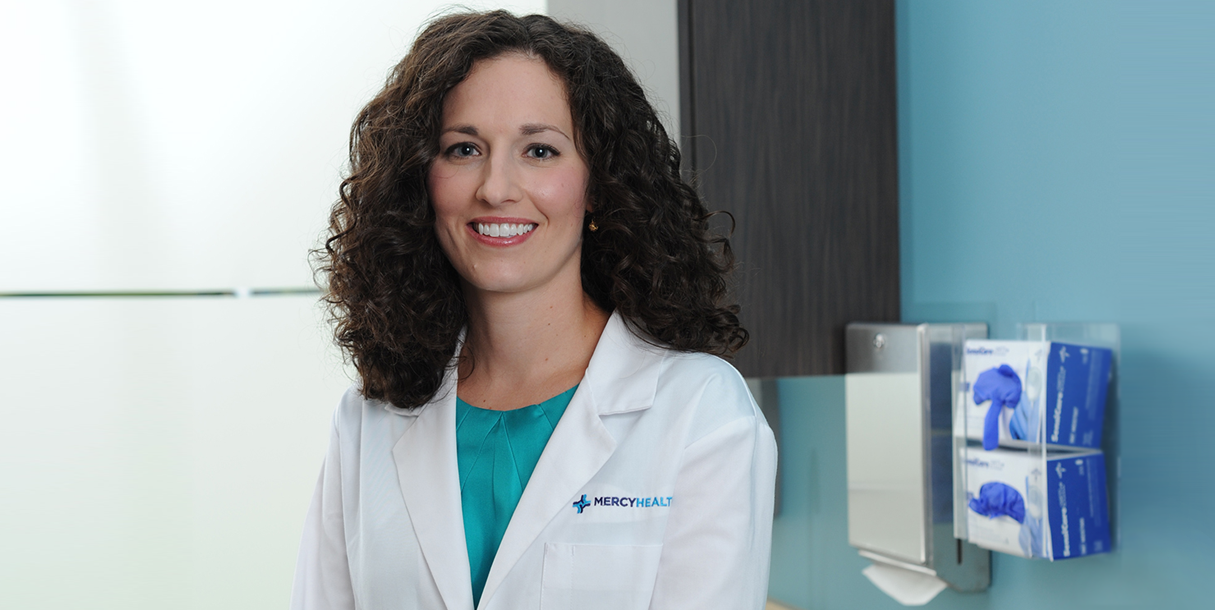
Summer is almost here and many of us eagerly anticipate the warmer weather and the sunshine it promises. It’s important to remember, however, that too much sunshine without proper protection can come at a price. Incidences of skin cancer are up and continue to grow annually. We talked with Mercy Health physician and dermatologist Emily Moosbrugger, MD about skin cancer prevention, cancer types, and everything under the sun when it comes to skin cancer.
Here’s everything you need to know about skin cancer prevention and treatment
How to prevent skin cancer
“Prevention remains the best strategy,” says Mercy Health physician and dermatologist Emily Moosbrugger, MD. “Use a sunscreen with an SPF of at least 30. Fifty is better. Reapply it every hour if you are swimming and every one to two hours to keep up with protection level on the bottle. You have to get a good enough layer on to benefit from sunscreen so don’t spread it too thin.”
What sunscreen to use
There are special sunscreens available for the face that minimize breakouts. Look for ones that are oil-free and non-comedogenic, meaning it won’t clog your pores. Water resistant options are best if you are swimming or taking part in activities that make you sweat. There are also sun protection hats on the market which can give you a sunscreen protection equivalent.
Who is more at-risk?
“People with fair skin, light eyes and light hair tend to burn easily and have more melanoma risk factors, as do people with a higher number of moles,” says Dr. Moosbrugger. “If this describes you, it’s even more important that you use sunscreen and use it properly.”
Early detection is the next line of defense for skin cancer prevention.
“Even if you are a low risk individual who doesn’t have too many moles, I recommend scheduling a baseline visit with dermatologist for a skin check,” says Dr. Moosbrugger. “Your dermatologist can work with you to determine a regular screening schedule that makes sense based on your risk level.”
Common types of skin cancer conditions
Actinic keratosis
The most common skin cancer condition that Dr. Moosbrugger sees is actinic keratosis, which are actually pre-cancerous lesions.
“Some of these lesions, which resemble rough scaly pink or red patches, never develop into anything serious but some can become squamous and basal cell carcinomas. That’s why we treat them,” says Dr. Moosbrugger.
Treatment options include:
- Freezing the lesions with liquid nitrogen in the dermatologist’s office
- Prescribing chemo cream that the patient takes home and applies on the lesion for couple of weeks
- Painting the lesion with medication and having the patient sit under sit under a special light that activates the medication
All of the treatment options cause the lesion to peel, inflame and then heal.
Basal cell carcinoma
Dr. Moosbrugger also commonly sees basal and squamous cell carcinomas, which are the next level up in severity from actinic keratosis.
“Basal cell carcinomas are small pink or white patches or bumps, similar to a pimple except that they don’t go away,” says Dr. Moosbrugger. “Once a biopsy confirms what it is, treatment options include curettage, or scraping, for superficial lesions located near the top layer of the skin. We treat bigger basal cell carcinomas with a scalpel, cutting around it before closing the wound with stitches. A pathologist confirms that the edges are clear on what we’ve removed.”
“If the basal cell carcinoma is on the head, neck, face or hands, we are likely to recommend that you see a Mohs surgeon, a dermatologist who’s completed a specialized fellowship in this type of microsurgery. With a Mohs procedure, the surgeon processes the tissue in the office as the procedure progresses, taking small layers of the carcinoma until it comes back clear before stitching you up. Mohs surgery has the highest cure rate and it spares tissue, providing a better cosmetic outcome.”
Left untreated, basal cell carcinomas will continue to grow or ulcerate down into the skin. In rare cases, they can even lead to death.
Squamous cell carcinoma
“Squamous cell carcinomas are not as common but they have more potential to spread. While they tend to be slow-growing, there is a subset of that can grow quickly. If caught early, they are low risk,” says Dr. Moosbrugger. “These appear as pink, scaly patches or bumps and tend to come up on sun-exposed areas. Again, we will biopsy the tissue to confirm what it is and treatment options are very similar to that for basal cell carcinomas.”
“Bigger or infiltrating squamous cell carcinomas sometimes call for Mohs surgery on parts of the body beyond the face. Radiation therapy is an option for advanced skin cancer or for an older patient who can’t tolerate surgery that a larger lesion would require.”
Melanoma
Melanoma is the most dangerous form of skin cancer and Dr. Moosbrugger sees more of them each year, in line with national trends.
“Melanomas can itch or bleed, appear various colors and often evolve over time. It’s important to check your skin regularly for anything that looks new and different. If you have a mole or other patch on your body that is asymmetric, has an irregular border, changes color, grows or evolves in any way, please get it checked,” she says.
The thickness of the melanoma determines the stage of the disease. Stage zero melanomas are those caught in top layer of the skin.
“If the melanoma is less than one millimeter thick in biopsy, we will excise it in the office. It goes to pathology to ensure the surrounding tissue is clear and if it is, the patient needs only to schedule continued screenings with a dermatologist,” says Dr. Moosbrugger. “If it measures more than one millimeter, we typically recommend a sentinel lymph node biopsy. This is a surgical procedure that is performed in the operating room. A surgical oncologist cuts out the melanoma as well as the lymph node to which it would drain to ensure the cancer hasn’t spread. If the lymph node is clear, the patient usually only needs continued frequent skin screenings. The patient is referred to an oncologist for additional care if not.”
When to check your skin
“If you have had a melanoma, check your skin monthly. Initially, you might see your dermatologist every three months and then build out to once or twice yearly as you remain cancer free. We recommend seeing most patients with other skin cancers every six to twelve months depending on the number and frequency of their skin cancers.”
“While we find some skin cancers where the sun doesn’t shine, the majority of them occur in sun-exposed areas,” notes Dr. Moosbrugger. “The sun damages cells cumulatively over time but luckily, it’s an environmental factor over which we can have some control.”
If you think you may need to check in with your doctor about skin cancer or want to learn more, visit the Mercy Health Skin Cancer page.