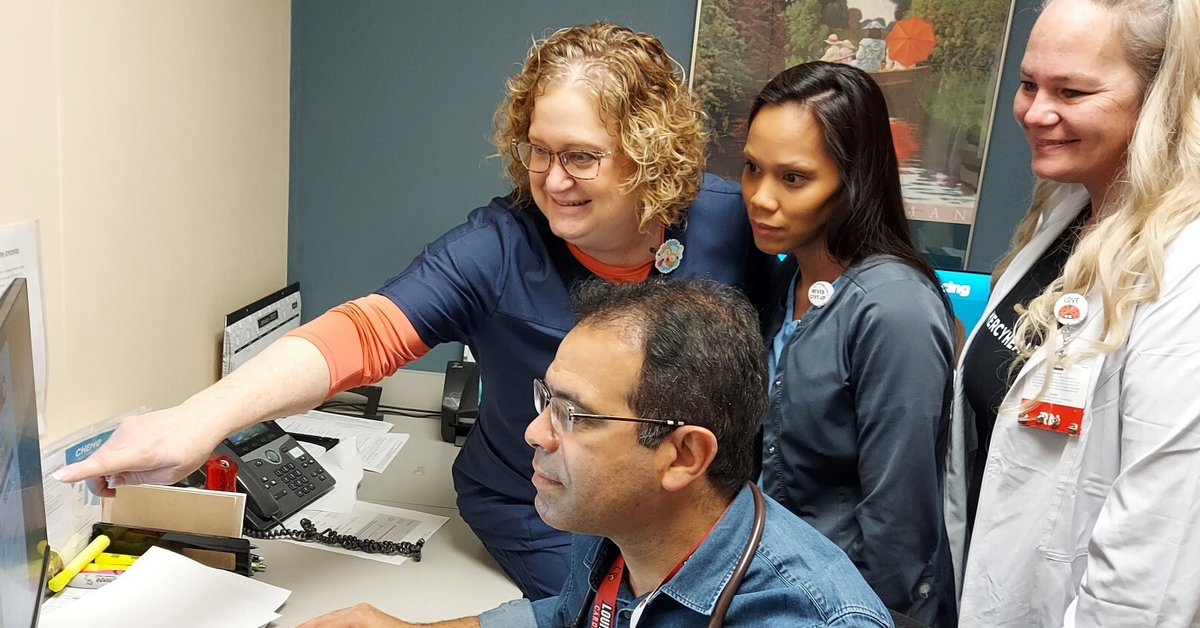
In 2020, Stephen Wilson, MD, (pictured above, right) of Mercy Health – Forest Park Internal Medicine, realized that some of his patients were struggling to manage their type 2 diabetes. From there, he and his medical practice care team set out to help them.
“We realized that we needed a multi-pronged approach to help patients living with diabetes achieve their health goals,” Dr. Wilson explains.
The result was the Forest Park Diabetes Management Program, winner of the Medical Fitness Association’s 2020 Program Innovation Award. This three-month program, funded by our ministry’s physicians, takes a comprehensive approach by looking at the interaction of diet, exercise and medicine and how they work together to impact blood sugar levels.
Dr. Wilson and his team recently graduated their third diabetes management program class, and with each group they’ve learned more about what can help patients lower their blood sugar long term.
“We’ve been excited to see consistency in the drop in patients’ A1C numbers and that the program, because of its comprehensiveness, works well for different age groups and demographics,” Dr. Wilson shares. “Our patients are primarily African American, and this program has worked well in a population which is medically underserved and understudied. It shows that lifestyle interventions work to manage diabetes. It’s just a matter of keeping people engaged.”
Dr. Wilson’s ultimate goal is to lower program patients’ A1C level to 7 or less. His initial group of 16 patients, with an average age of 51, dropped an average of 1.48 points to a measure of 9.9 at the end of the program. All patients in this group were and remained on diabetes medication.
“A few got close to the goal or exceeded it,” he says. “Those who were most engaged in all aspects of the program did the best.”
The second group had 12 participants and had an older average age. Their starting average A1C was lower, but the drop in numbers by the end of the program was about the same.
“They were more successful,” Dr. Wilson says. “They started with a lower average number and managed to drop their numbers even then. The lower A1C level you get, the harder it is to lose a good amount. Again, some participants reached or exceeded the goal to get to 7 and as a result, some got to reduce their medication intake.”
And with this most recent third set of patients, the program added some new free elements: a visit with a dietitian, gym access, fresh produce through the Produce Perks delivery program and access to a psychologist to help patients develop strategies to stay on course.
“One patient was in good shape but drank two liters of soda a day,” Dr. Wilson tells. “But meeting with the dietitian led to a big drop in that patient’s A1C numbers.”
Group exercise helped participants build community, but at the program’s end, some patients were unable to keep up a gym membership due to cost.
“In losing that framework, some have slipped a bit in maintaining an exercise routine,” Dr. Wilson notes.
Additionally, behavioral support turned out to be crucial in the management of chronic illness.
“Many patients had some anxiety or mood disorder when they started the program,” Dr. Wilson shares. “That can lead to binge eating, and addressing that and helping them understand why they were eating helped with their glycemic control.”
Access to healthy foods was also key.
“Being able to access fresh produce goes a long way to improve health,” Dr. Wilson says. “Patients were curious about how to prepare food in a healthier manner. Through Produce Perks, they received items like zucchini, squash, bell peppers, different greens and fruits every two weeks and we provided them with recipes.”
The last group of patients was younger than the first two groups and they, too, made good progress in lowering their A1C numbers.
“Investing in lifestyle interventions, such as dietary education and access to produce as well as places to move, can impact how diabetes is controlled and improve outcomes for diabetes,” Dr. Wilson concludes. “When you take a comprehensive approach to managing diabetes, people will latch onto what they like and continue to follow the program.”
Going forward, Dr. Wilson is looking at other elements to investigate.
“We still need to look at the impact of blood sugar on weight loss, blood pressure and eating habits, as well as continued access to exercise and a dietitian for continuing support. Also, when patients get more consistent feedback, on their blood sugar, they change their behavior. But it’s hard to ask to stick yourself four times a day. Continuous feedback sensors give constant feedback and studies show that leads to behavior change. We will allow all patients with diabetes to get one of these monitors at no cost and see what success we have.”
Learn more about the diabetes management and care services we offer at Mercy Health.